Even with the best protocols in place, treating COVID-19 patients is inherently dangerous for health professionals. But what if there was a way to monitor patients from a safe distance?
This week a clinical team in Boston has reported being able to monitor a COVID-19 patient remotely, thanks to a device developed at MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) that can monitor a patient’s breathing, movement and sleep patterns using wireless signals.
The CSAIL team’s device, which they call “Emerald,” has been used in multiple hospitals and assistive-care facilities, including with a COVID-19 patient at Heritage Assisted Living in the Boston suburb of Framingham.
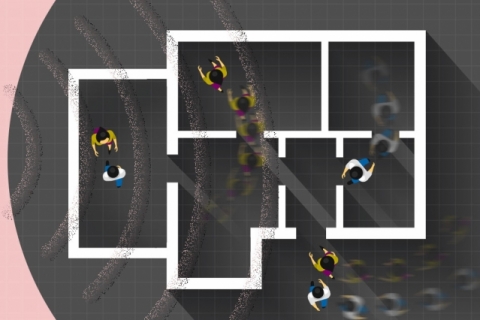
Developed by MIT professor Dina Katabi and her research group at CSAIL, Emerald is a WiFi-like box that analyzes the wireless signals in the environment using artificial intelligence to infer people’s vital signs, sleep, and movement. (The signals emit roughly 1000 times less radiation than a standard cellphone.)
After obtaining consent, Heritage installed Emerald in the patient's room, where it non-invasively monitors her health and reports the data to her doctor, Ipsit Vahia. Sitting in his home, Dr. Vahia can remotely track the patient’s progress by looking at metrics like breathing and walking speed.
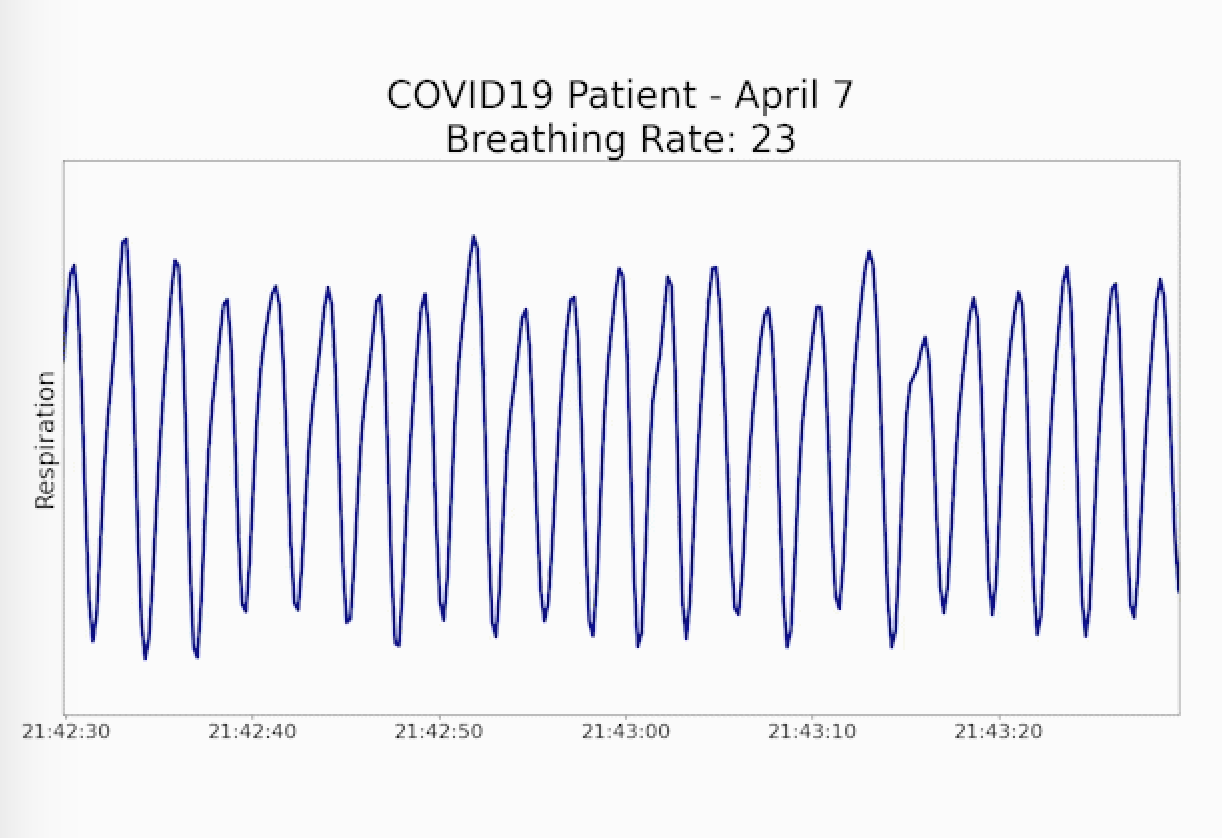
Specifically, Emerald data showed that the patient’s initial breathing rate had gone down from 23 to 18 breaths per minute - much closer to the patient’s baseline. The system also showed that the patient's sleep quality improved, and that she was able to walk more quickly around her apartment as she recovered.

“When doctors have to interact directly with patients to conduct exams or monitor vital signs, each step along the way represents an increased risk that they will get infected,” says Vahia, an assistant professor of psychiatry at Harvard Medical School. “Given how Emerald can generate important health data without any patient contact, it could minimize the risk that doctors and nurses will catch the disease from their patients.”
Emerald could also help detect other respiratory problems that would otherwise go unnoticed. Vahia has used Emerald with a patient who suffers from anxiety and has insomnia problems. Emerald’s data predicted that the patient had sleep apnea, which was confirmed with follow-up testing.
Katabi and her team have worked with hospitals, nursing homes, and pharmaceutical companies on remote health monitoring. She says that COVID-19 is particularly challenging for assisted living facilities and retirement homes, since they have vulnerable populations who already have other diseases.
“It’s clear that, with these high-risk elderly patients, they would greatly benefit from us being able to passively gather medical data over time when it is not possible to interface with each person directly,” says William McGrory, who oversees mental health services for Heritage Assisted Living. Heritage is also currently conducting a pilot project using Emerald that’s focused on assessing dementia.
Beyond the immediate doctor-patient interaction, Katabi says that remote-sensing devices like Emerald could assist in expanding healthcare capacity. As the demand on hospitals spikes with the increasing number of COVID-19 patients, Emerald’s safe remote and detailed health monitoring could allow hospitals and physicians to triage less severe patients and monitor them in their own homes, while still allowing them to respond quickly in case of aggravated illness.
Vahia says that COVID-19 has already spurred a monumental shift in getting medical professionals to explore technological solutions for providing care from a distance.
“Even in just the last few weeks, there’s been a newfound urgency about developing remote-sensing technologies like Emerald that can help doctors do their jobs as safely as possible,” says Vahia, who also directs McLean Hospital's Technology and Aging Laboratory, which studies how digital tools can impact elder care.